Introduction Dealing with diarrhea can be exhausting, especially if it’s caused by Clostridioides difficile (C. diff), a bacterial infection affecting nearly 500,000 Americans annually. While diarrhea is a common ailment, C. diff infection can lead to severe complications, including life-threatening inflammation of the colon. Understanding how C. diff spreads, its symptoms, and who is most
Introduction
Dealing with diarrhea can be exhausting, especially if it’s caused by Clostridioides difficile (C. diff), a bacterial infection affecting nearly 500,000 Americans annually. While diarrhea is a common ailment, C. diff infection can lead to severe complications, including life-threatening inflammation of the colon. Understanding how C. diff spreads, its symptoms, and who is most vulnerable is crucial for effective prevention and management.
How C. diff Spreads
C. diff, like many bacteria, is present in stool and can survive on surfaces, including our skin and shoes. However, it remains inactive in the form of spores until it reaches the intestines. Only then do favorable conditions allow the spores to germinate and become active, leading to infection. This typically occurs when the balance of the gut microbiome is disrupted, allowing C. diff to proliferate and release toxins that cause illness.
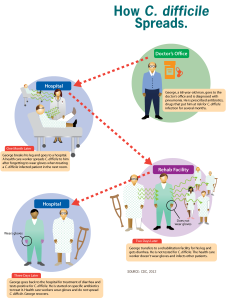
Image by: yendex.com
Symptoms of C. diff Infection
Recognizing the symptoms of C. diff infection is essential for prompt diagnosis and treatment. While symptoms can vary in severity, common signs include:
- Persistent diarrhea lasting three or more days
- Nausea
- Fever
- Stomach pain or tenderness
- Loss of appetite
It’s important to note that these symptoms may overlap with other gastrointestinal ailments, making diagnosis challenging, especially in the early stages of infection. However, individuals who have recently taken antibiotics or have been in close contact with someone diagnosed with C. diff should be particularly vigilant for these symptoms.
Vulnerable Populations
Certain groups are at higher risk of developing C. diff infection, including:
- Individuals undergoing antibiotic therapy or who have recently completed a course of antibiotics
- Those with weakened immune systems due to conditions such as cancer, organ transplant, or autoimmune disorders
- People in close contact with individuals diagnosed with C. diff, especially in healthcare settings
While C. diff infections have traditionally been associated with healthcare facilities like hospitals and nursing homes, there is a growing concern about community-based infections occurring among the general population. This highlights the need for increased awareness and preventive measures beyond healthcare settings.
Prevention Strategies
Preventing C. diff infection requires a multi-faceted approach, involving both healthcare institutions and individuals. Hospitals and healthcare facilities implement strict hygiene protocols, including frequent handwashing and isolation of infected patients, to prevent the spread of the bacteria.
Outside of healthcare settings, individuals can take several steps to reduce their risk of C. diff infection:
- Thorough handwashing with soap and water, especially after using the bathroom and before eating
- Avoiding unnecessary antibiotic use and discussing alternatives with healthcare providers
- When antibiotics are necessary, opting for narrow-spectrum antibiotics when appropriate to minimize disruption of the gut microbiome
- Disinfecting surfaces and maintaining cleanliness, particularly in households where someone has been diagnosed with C. diff

Photo by: www.pexels.com
Comparison of Antibiotics
Not all antibiotics carry the same risk of C. diff infection. Recent research has identified certain antibiotics that pose a higher risk, including clindamycin and later-generation cephalosporins, while others have a lower risk, such as minocycline and doxycycline. Healthcare providers should consider these risks when prescribing antibiotics and explore alternative options when feasible. Explore More About (Immune Boosts)
| Antibiotic | Risk for C. diff Infection |
|---|---|
| Clindamycin | High |
| Later-generation cephalosporins | High |
| Minocycline | Low |
| Doxycycline | Low |
Role of Probiotics
Probiotics, which are live microorganisms found in supplements, yogurt, and other fermented foods, have been suggested as a potential way to support gut health and prevent C. diff infection. However, research on their effectiveness in preventing or treating C. diff infection is inconclusive. While probiotics may aid in microbiome recovery after antibiotic therapy, their use should be approached with caution, as they may delay recovery in some cases.
Treatment of C. diff Infection
Treatment for C. diff infection typically involves antibiotics, despite the irony of using antibiotics to combat a bacterial infection exacerbated by antibiotic use. Fidaxomicin and oral vancomycin are commonly prescribed antibiotics for C. diff infection. However, approximately one in five individuals will experience one or more recurrences of the infection, highlighting the need for alternative treatment approaches.
In cases of recurrent C. diff infection, fecal microbial transplantation (FMT) has emerged as a promising treatment option. FMT involves transferring fecal matter from a healthy donor into the patient’s gut, restoring microbial balance and combating C. diff colonization. Additionally, the FDA has approved live fecal microbiota products aimed at preventing recurrent C. diff infections, offering hope for those struggling with persistent illness.
Conclusion
C. diff infection poses a significant healthcare challenge, affecting thousands of individuals each year and causing severe morbidity and mortality. While antibiotics remain a cornerstone of treatment, prevention strategies, including prudent antibiotic use, thorough hand hygiene, and targeted interventions, are essential for reducing the burden of C. diff infection. Continued research into alternative treatment approaches, such as FMT and probiotics, offers hope for improved outcomes and quality of life for those affected by this debilitating illness.