In recent years, the scientific community has increasingly acknowledged the profound and intricate relationship between the gut and the brain, often referred to as the Gut-Brain Connection. This bidirectional communication system, involving a complex interplay of neural, hormonal, and immunological pathways, has far-reaching implications for our understanding of health and disease. Emerging research is shedding
In recent years, the scientific community has increasingly acknowledged the profound and intricate relationship between the gut and the brain, often referred to as the Gut-Brain Connection. This bidirectional communication system, involving a complex interplay of neural, hormonal, and immunological pathways, has far-reaching implications for our understanding of health and disease. Emerging research is shedding light on how this connection influences not only gastrointestinal function but also mental health, cognition, and overall well-being.
The Anatomy of the Gut-Brain Connection
The Gut-Brain Connection is facilitated by the gut-brain axis, a communication network linking the central nervous system (CNS) with the enteric nervous system (ENS). The ENS, often dubbed the “second brain,” contains approximately 100 million neurons embedded in the walls of the gastrointestinal tract. This extensive neural network allows the gut to operate semi-autonomously, managing digestion and interacting with the CNS via the vagus nerve and other neural pathways.
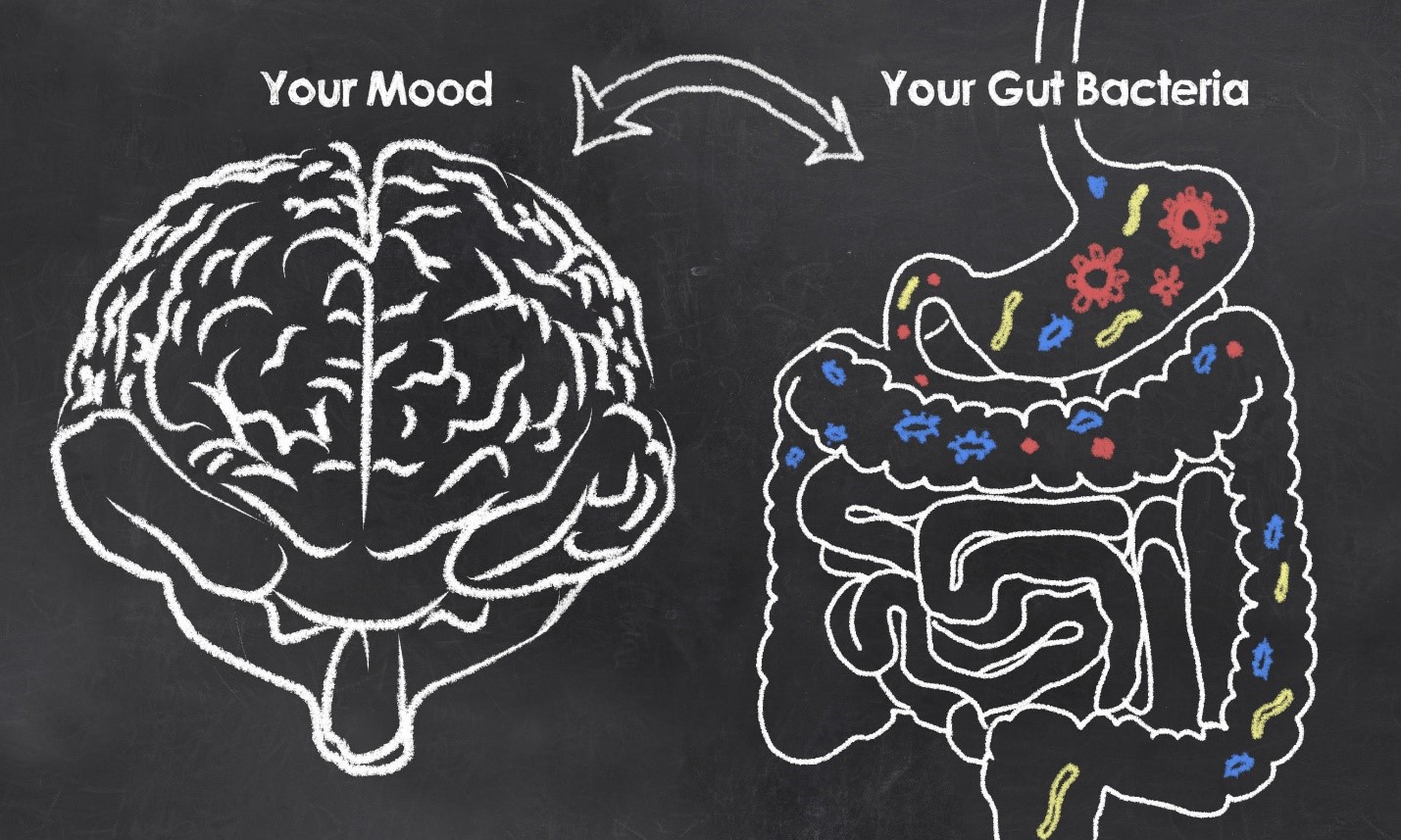
Additionally, the gut-brain axis includes endocrine signaling through hormones such as ghrelin and leptin, which regulate appetite and energy balance, and immune signaling through cytokines and other inflammatory mediators. The gut microbiota, a diverse community of trillions of microorganisms residing in the intestines, also plays a crucial role in this connection by producing neurotransmitters and other bioactive compounds that influence brain function.
The Role of the Microbiota
The gut microbiota is a key player in the Gut-Brain Connection. These microorganisms produce a variety of substances, including short-chain fatty acids (SCFAs), neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), and metabolites that can cross the blood-brain barrier. SCFAs, such as butyrate, propionate, and acetate, are produced through the fermentation of dietary fibers and have been shown to have anti-inflammatory properties and influence brain function.
Serotonin, often called the “feel-good” neurotransmitter, is predominantly produced in the gut, with about 90% of the body’s serotonin being synthesized by enterochromaffin cells in the gastrointestinal tract. This gut-derived serotonin plays a role in regulating mood, anxiety, and even intestinal motility.
The composition and diversity of the gut microbiota can be influenced by various factors, including diet, antibiotics, stress, and lifestyle. Dysbiosis, an imbalance in the gut microbiota, has been linked to a range of conditions, from irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) to neuropsychiatric disorders like depression, anxiety, and autism spectrum disorders.
Mental Health and the Gut-Brain Connection
One of the most intriguing aspects of the Gut-Brain Connection is its impact on mental health. Numerous studies have suggested a link between gut health and mental well-being, with alterations in the gut microbiota being associated with conditions such as depression, anxiety, and stress-related disorders.
For instance, a study published in the journal Nature Microbiology found that individuals with depression had a distinct gut microbiota composition compared to healthy controls. The researchers identified specific bacterial genera that were depleted or enriched in depressed individuals, suggesting that these microbes may play a role in the pathophysiology of depression.
Moreover, animal studies have demonstrated that manipulating the gut microbiota can influence behavior and brain chemistry. Germ-free mice, which lack a gut microbiota, exhibit altered stress responses and cognitive deficits. When these mice are colonized with microbiota from healthy animals, their behavior and brain function normalize, highlighting the importance of the gut microbiota in regulating mental health.
Picture by: Yandex.com
Cognitive Function and the Gut-Brain Connection
Beyond mental health, the Gut-Brain Connection also appears to play a role in cognitive function. Research has shown that the gut microbiota can influence learning, memory, and decision-making processes. For example, a study published in the journal Brain, Behavior, and Immunity found that mice treated with probiotics exhibited improved performance in memory tasks and had increased levels of brain-derived neurotrophic factor (BDNF), a protein involved in neuroplasticity and cognitive function.
In humans, a pilot study published in Frontiers in Aging Neuroscience investigated the effects of a probiotic supplement on cognitive function in older adults. The researchers found that participants who received the probiotic showed improvements in cognitive performance and had changes in gut microbiota composition, suggesting a potential link between gut health and cognitive aging.
Therapeutic Potential
The growing body of evidence supporting the Gut-Brain Connection has opened up new avenues for therapeutic interventions. Probiotics, prebiotics, and dietary interventions are being explored as potential treatments for a range of conditions, from gastrointestinal disorders to mental health issues and neurodegenerative diseases.
Probiotics, which are live microorganisms that confer health benefits when consumed in adequate amounts, have shown promise in modulating the gut microbiota and improving symptoms of IBS, depression, and anxiety. Prebiotics, which are non-digestible fibers that selectively stimulate the growth of beneficial bacteria, may also have a positive impact on gut health and the Gut-Brain Connection.
Dietary interventions, such as the Mediterranean diet, have been associated with improved gut microbiota composition and reduced risk of depression and cognitive decline. This diet, rich in fruits, vegetables, whole grains, and healthy fats, provides essential nutrients and fibers that support a healthy gut microbiota and overall well-being.
Future Directions
While the research on the Gut-Brain Connection is still in its early stages, the findings to date are promising and suggest that this connection plays a crucial role in health and disease. Future studies will need to further elucidate the mechanisms underlying the Gut-Brain Connection and explore how individual differences in genetics, lifestyle, and environment influence this relationship.
Moreover, large-scale clinical trials are needed to validate the therapeutic potential of interventions targeting the gut microbiota. Personalized approaches, taking into account an individual’s unique gut microbiota composition and health status, may offer the most effective strategies for harnessing the power of the Gut-Brain Connection.
Conclusion
The Gut-Brain Connection represents a fascinating and rapidly evolving field of research with significant implications for our understanding of health and disease. By unraveling the complex interactions between the gut and the brain, scientists are uncovering new insights into the role of the gut microbiota in mental health, cognitive function, and overall well-being. As research continues to advance, the potential for novel therapeutic interventions targeting the Gut-Brain Connection holds great promise for improving health outcomes and enhancing quality of life.