In recent years, healthcare accessibility and affordability have become critical topics of discussion among policymakers, healthcare providers, and the general public. The confluence of technological advancements, policy reforms, and evolving patient expectations has led to significant transformations within the healthcare landscape. This article delves into the current trends shaping healthcare accessibility and affordability, examining their
In recent years, healthcare accessibility and affordability have become critical topics of discussion among policymakers, healthcare providers, and the general public. The confluence of technological advancements, policy reforms, and evolving patient expectations has led to significant transformations within the healthcare landscape. This article delves into the current trends shaping healthcare accessibility and affordability, examining their implications for the future.
Telehealth and Digital Health Solutions
One of the most significant trends in healthcare accessibility is the rise of telehealth and digital health solutions. The COVID-19 pandemic accelerated the adoption of telehealth, allowing patients to receive medical consultations and treatments remotely. This shift has not only increased accessibility for individuals in rural and underserved areas but also reduced the burden on healthcare facilities.
Digital health solutions, including mobile health apps and wearable devices, have further enhanced patient engagement and self-management of chronic conditions. These technologies enable continuous monitoring and real-time data sharing between patients and healthcare providers, leading to more personalized and timely care. As telehealth becomes more integrated into standard practice, it is expected to play a pivotal role in improving healthcare accessibility and affordability.
Value-Based Care Models
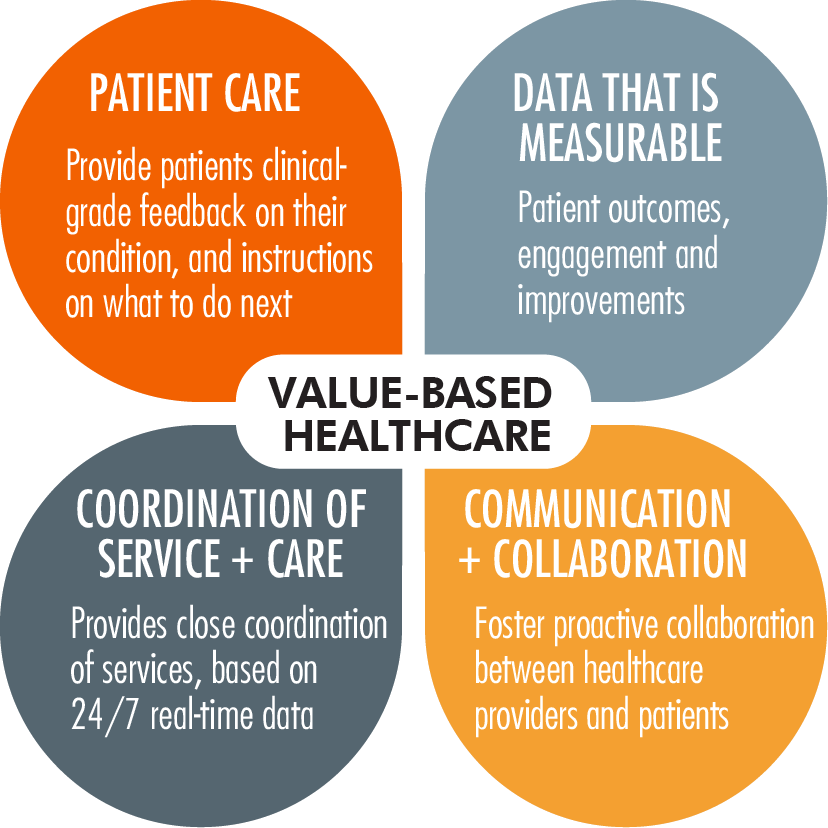
The transition from fee-for-service to value-based care models represents a paradigm shift in healthcare delivery. Value-based care focuses on patient outcomes rather than the volume of services provided. This approach incentivizes healthcare providers to deliver high-quality, cost-effective care, ultimately improving patient satisfaction and reducing healthcare costs.
Accountable Care Organizations (ACOs) and bundled payment models are examples of value-based care initiatives that have gained traction. These models encourage collaboration among healthcare providers, streamline care coordination, and reduce unnecessary hospitalizations and procedures. By aligning financial incentives with patient outcomes, value-based care models hold promise for enhancing both accessibility and affordability in the healthcare system.
Policy Reforms and Government Initiatives
Government policies and initiatives play a crucial role in shaping healthcare accessibility and affordability. The Affordable Care Act (ACA) in the United States, for instance, expanded Medicaid coverage and established health insurance marketplaces, increasing access to healthcare for millions of Americans. While the ACA has faced challenges and political debates, its impact on healthcare accessibility cannot be understated.
Globally, governments are implementing various reforms to address healthcare disparities and improve affordability. Universal health coverage (UHC) initiatives aim to provide all individuals with access to essential health services without financial hardship. Countries like Canada, the United Kingdom, and Australia have long-standing UHC systems, while others are working towards achieving this goal.
Picture by: Yandex.com
Pharmaceutical Pricing and Transparency
The rising cost of prescription drugs remains a significant barrier to healthcare affordability. In response, there is a growing emphasis on pharmaceutical pricing transparency and regulation. Policymakers are advocating for measures such as price caps, increased competition through generic drugs, and greater negotiation power for government programs like Medicare.
Additionally, initiatives like the 340B Drug Pricing Program in the United States aim to provide discounted medications to eligible healthcare organizations, ultimately benefiting low-income and uninsured patients. Transparent pricing and regulatory efforts are essential to ensuring that life-saving medications remain accessible and affordable for all individuals.
Health Insurance Innovations
Innovations in health insurance are also contributing to improved healthcare accessibility and affordability. High-deductible health plans (HDHPs) paired with Health Savings Accounts (HSAs) offer individuals greater control over their healthcare spending. These plans encourage consumers to make informed decisions about their healthcare needs while providing tax advantages for saving and paying for medical expenses.
Moreover, value-based insurance design (VBID) is gaining popularity as a strategy to align insurance benefits with the value of services provided. VBID plans reduce or eliminate cost-sharing for high-value services, such as preventive care and chronic disease management, while maintaining cost-sharing for low-value services. This approach promotes the use of effective healthcare services and reduces overall healthcare costs.
Addressing Social Determinants of Health
Recognizing the impact of social determinants of health (SDOH) on healthcare accessibility and affordability is crucial for creating a more equitable healthcare system. SDOH, including factors like income, education, housing, and transportation, significantly influence an individual’s ability to access and afford healthcare services.
Healthcare organizations and policymakers are increasingly focusing on addressing SDOH through community-based interventions and partnerships. For example, programs that provide housing assistance, food security, and transportation services can improve health outcomes and reduce healthcare costs. By addressing the root causes of health disparities, these initiatives contribute to a more accessible and affordable healthcare system.
The Role of Artificial Intelligence and Big Data
Artificial intelligence (AI) and big data analytics are revolutionizing healthcare by enhancing diagnostic accuracy, predicting disease outbreaks, and optimizing resource allocation. AI-powered tools can analyze vast amounts of data to identify patterns and trends, enabling early intervention and personalized treatment plans.
Big data analytics also play a role in identifying inefficiencies within the healthcare system, leading to cost-saving measures and improved accessibility. For instance, predictive analytics can forecast patient demand, allowing healthcare providers to allocate resources more effectively and reduce wait times. As AI and big data continue to evolve, their potential to enhance healthcare accessibility and affordability will only grow.
Conclusion
The landscape of healthcare accessibility and affordability is undergoing a transformative shift, driven by technological advancements, policy reforms, and a focus on value-based care. Telehealth, digital health solutions, and AI are revolutionizing patient care, while government initiatives and insurance innovations are addressing long-standing barriers to access and affordability. By addressing social determinants of health and promoting transparency in pharmaceutical pricing, stakeholders are working towards a more equitable and sustainable healthcare system.
As these trends continue to evolve, collaboration among policymakers, healthcare providers, and technology innovators will be essential to ensuring that healthcare remains accessible and affordable for all individuals. The future of healthcare lies in a holistic approach that prioritizes patient outcomes, embraces technological advancements, and addresses the social factors influencing health.
















