Asthma is a chronic respiratory condition that affects millions of people worldwide. Characterized by inflammation and narrowing of the airways, asthma can cause symptoms such as wheezing, shortness of breath, chest tightness, and coughing. For many, these symptoms can significantly impact daily life, making even simple activities a challenge. Fortunately, advancements in asthma treatments are
Asthma is a chronic respiratory condition that affects millions of people worldwide. Characterized by inflammation and narrowing of the airways, asthma can cause symptoms such as wheezing, shortness of breath, chest tightness, and coughing. For many, these symptoms can significantly impact daily life, making even simple activities a challenge. Fortunately, advancements in asthma treatments are offering new hope and improving the quality of life for those affected by this condition.
Traditional Asthma Treatments
Before diving into the latest advancements, it is essential to understand the traditional treatments for asthma. Historically, asthma management has relied on two main types of medications: quick-relief (or rescue) inhalers and long-term control medications.
- Quick-Relief Inhalers: These inhalers, often containing short-acting beta-agonists like albuterol, provide rapid relief from acute asthma symptoms. They are essential during an asthma attack but do not address the underlying inflammation.
- Long-Term Control Medications: These include inhaled corticosteroids, long-acting beta-agonists, leukotriene modifiers, and theophylline. These medications aim to reduce airway inflammation and prevent asthma attacks when used regularly.
While these treatments have been effective for many, they are not without limitations. Some patients experience side effects, and others find that their symptoms are not adequately controlled. This has led to the development of new asthma treatments that offer more targeted and personalized approaches.
Biologic Therapies: A New Frontier
One of the most exciting advancements in asthma treatments is the development of biologic therapies. Biologics are medications derived from living cells that target specific molecules involved in the inflammatory process of asthma. These treatments are particularly beneficial for individuals with severe asthma that is not well-controlled with traditional medications.
- Omalizumab (Xolair): This biologic targets immunoglobulin E (IgE), a molecule involved in allergic asthma. By binding to IgE, omalizumab reduces allergic reactions and asthma symptoms.
- Mepolizumab (Nucala) and Reslizumab (Cinqair): These biologics target interleukin-5 (IL-5), a cytokine involved in the production and survival of eosinophils, a type of white blood cell that contributes to inflammation in asthma. By reducing eosinophil levels, these treatments help control severe eosinophilic asthma.
- Benralizumab (Fasenra): This biologic also targets IL-5 but works by binding to the IL-5 receptor on eosinophils, leading to their destruction. This results in a significant reduction in eosinophil levels and improved asthma control.
- Dupilumab (Dupixent): This biologic targets the IL-4 and IL-13 pathways, which are involved in both allergic and eosinophilic asthma. By blocking these pathways, dupilumab helps reduce inflammation and improve lung function.
Biologic therapies have shown remarkable efficacy in clinical trials, with many patients experiencing fewer asthma attacks, reduced symptoms, and improved lung function. These treatments are administered via injection, typically every few weeks, and are tailored to the specific type of asthma a patient has, making them a more personalized approach to asthma management.
Picture by: Yandex.com
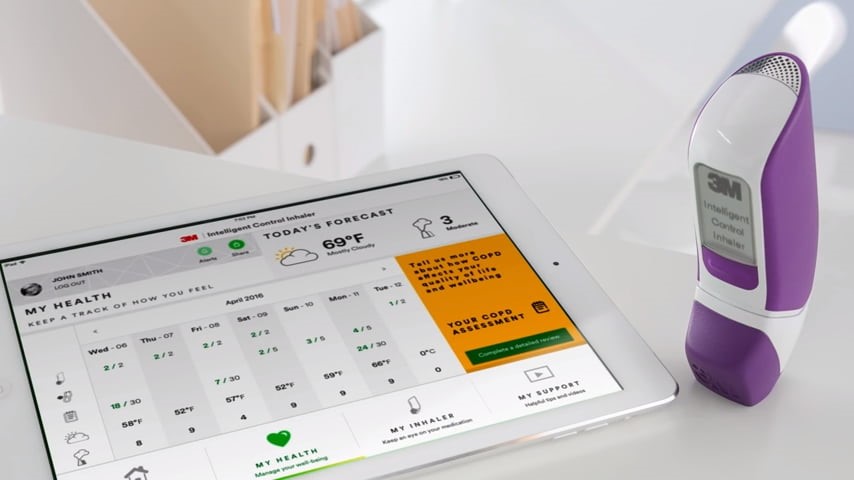
Advances in Inhaler Technology
Inhalers are a cornerstone of asthma treatment, and recent advancements in inhaler technology have further improved their effectiveness and ease of use.
- Smart Inhalers: These devices are equipped with sensors that track inhaler usage and provide feedback to patients and healthcare providers. By monitoring adherence and technique, smart inhalers help ensure that patients are using their medications correctly, which can lead to better asthma control.
- Dry Powder Inhalers (DPIs): Unlike traditional metered-dose inhalers (MDIs) that require coordination between inhalation and actuation, DPIs deliver medication in a dry powder form that is easier to inhale. This can be particularly beneficial for individuals with difficulty using MDIs.
- Soft Mist Inhalers (SMIs): SMIs create a slow-moving mist that allows for more efficient delivery of medication to the lungs. This technology can improve drug deposition and reduce the need for high doses, potentially minimizing side effects.
Personalized Asthma Management
The concept of personalized medicine is gaining traction in asthma treatment. By tailoring treatments to an individual’s specific type of asthma, healthcare providers can achieve better outcomes. This approach involves several key components:
- Phenotyping and Biomarkers: Identifying the specific phenotype of asthma (e.g., allergic, eosinophilic, non-eosinophilic) and using biomarkers (e.g., blood eosinophil levels, FeNO) helps guide treatment decisions. This ensures that patients receive the most appropriate therapies for their condition.
- Genetic Testing: Advances in genetic testing are allowing researchers to identify genetic variations that influence asthma severity and response to treatment. This information can be used to develop more targeted therapies and predict which patients are likely to benefit from specific treatments.
- Patient Education and Self-Management: Empowering patients with knowledge about their condition and how to manage it is crucial for improving asthma control. This includes education on proper inhaler technique, recognizing and avoiding triggers, and developing an asthma action plan.
The Role of Telemedicine
Telemedicine has become an invaluable tool in asthma management, particularly during the COVID-19 pandemic. Virtual consultations allow healthcare providers to monitor patients remotely, adjust treatment plans, and provide education and support. This approach can improve access to care, especially for individuals in remote or underserved areas.
Future Directions
The future of asthma treatment is promising, with ongoing research and development aimed at finding even more effective and personalized therapies. Some areas of focus include:
- Gene Therapy: Researchers are exploring the potential of gene therapy to correct genetic defects that contribute to asthma. While still in the early stages, this approach holds the promise of a long-term cure for certain types of asthma.
- Microbiome Research: The gut and lung microbiomes play a role in immune function and inflammation. Understanding how these microbial communities influence asthma could lead to new treatments that target the microbiome.
- New Biologics and Small Molecules: Scientists are continually developing new biologics and small molecule drugs that target different pathways involved in asthma. These treatments may offer additional options for patients who do not respond to existing therapies.
Conclusion
Advancements in asthma treatments are transforming the lives of individuals with this chronic condition. From biologic therapies and innovative inhaler technologies to personalized medicine and telemedicine, these new approaches are providing better symptom control, fewer asthma attacks, and improved overall quality of life. As research continues to uncover new insights and develop novel therapies, the future looks bright for those living with asthma.
















