Introduction Chikungunya Virus, a viral disease transmitted by mosquitoes, poses a significant global health concern. The causative agent, Chikungunya virus (CHIKV), belongs to the alphavirus genus in the Togaviridae family, specifically an RNA virus. The word “chikungunya” originates from the Kimakonde language, signifying “to become contorted.” This term aptly describes the characteristic joint pain associated
Introduction
Chikungunya Virus, a viral disease transmitted by mosquitoes, poses a significant global health concern. The causative agent, Chikungunya virus (CHIKV), belongs to the alphavirus genus in the Togaviridae family, specifically an RNA virus. The word “chikungunya” originates from the Kimakonde language, signifying “to become contorted.” This term aptly describes the characteristic joint pain associated with the disease.
Distribution and Outbreaks
The history of CHIKV dates back to its identification in 1952 in the United Republic of Tanzania. Subsequently, it has spread across Africa and Asia, with notable urban outbreaks recorded in Thailand (1967) and India (1970s). Since 2004, CHIKV outbreaks have become more frequent and widespread, partly due to viral adaptations that enhance transmission by Aedes albopictus mosquitoes. The virus has now been identified in over 110 countries spanning Asia, Africa, Europe, and the Americas.
Transmission often persists in countries where a large portion of the population remains susceptible to the virus. Regions with established populations of Aedes aegypti or Aedes albopictus mosquitoes have experienced local mosquito-borne transmission.

Image by: yendex.com
Transmission
The primary vectors for Chikungunya Virus transmission are Aedes (Stegomyia) aegypti and Aedes (Stegomyia) albopictus, the same mosquitoes responsible for spreading dengue and Zika viruses. These mosquitoes exhibit daytime biting behavior and lay their eggs in containers with standing water. Ae. aegypti also feeds indoors.
When an uninfected mosquito feeds on a person with circulating CHIKV in their blood, the virus is ingested. Subsequently, the virus replicates in the mosquito, reaching its salivary glands. The virus can then be transmitted to a new human host when the mosquito bites again, restarting the transmission cycle.

Image by: yendex.com
Symptoms
In Symptomatic Patients:
- Onset: Typically 4–8 days (range 2–12 days) after an infected mosquito bite.
- Fever: Abrupt onset, often accompanied by severe joint pain.
- Joint Pain: Frequently debilitating, lasting for days, weeks, months, or even years.
- Other Common Signs: Joint swelling, muscle pain, headache, nausea, fatigue, and rash.
In Asymptomatic Patients:
- Mild Symptoms: In the absence of significant joint pain, symptoms are usually mild.
- Risk of Misdiagnosis: Overlapping symptoms with dengue and Zika viruses may lead to misdiagnosis.
Complications:
- Eye, Heart, Neurological Complications: Occasional cases reported.
- Age-Related Risk: Patients at extremes of age (newborns and older individuals with underlying conditions) are at higher risk of severe disease.
Post-Recovery:
- Likely Immunity: Evidence suggests recovered individuals are likely immune from future infections.
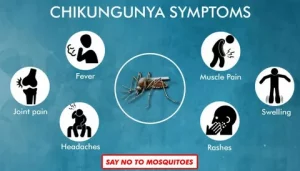
Image by: yendex.com
Diagnostics
Chikungunya virus can be detected directly in blood samples collected during the first week of illness using tests like reverse transcriptase–polymerase chain reaction (RT–PCR). Additionally, tests measuring the immune response, such as antibody tests, are used after the first week to detect antibodies to the virus. These antibodies remain detectable for about two months.
Treatment and Vaccines
Clinical Management:
- Symptomatic Treatment: Addressing fever and joint pain with anti-pyretics and optimal analgesics.
- Fluids and Rest: Drinking plenty of fluids and getting adequate rest.
Medications:
- Paracetamol or Acetaminophen: Recommended for pain relief and reducing fever.
- Caution with NSAIDs: Non-steroidal anti-inflammatory drugs (NSAIDs) avoided until dengue infections are ruled out due to increased bleeding risk.
Vaccines (as of Dec 2022):
- In Development: Several vaccines are in different stages of development.
- No Licensed Vaccine: Despite ongoing efforts, no commercial vaccine is available for CHIKV.
Prevention and Control
Primary Prevention:
- Avoiding Mosquito Bites: Key to protection.
- Protective Clothing: Minimize skin exposure during outbreaks.
- Window and Door Screens: Prevent mosquitoes from entering homes.
- Repellents: Apply to exposed skin or clothing, containing DEET, IR3535, or icaridin.
Vector Control:
- Community Mobilization: Critical for reducing mosquito breeding sites.
- Insecticides: Sprayed during outbreaks to kill adult mosquitoes.
- Larvae Control: Applied to surfaces and water in containers to kill immature larvae.
During Outbreaks:
- Protective Measures: Insecticide-treated nets, appropriate clothing, and repellents advised.
Travel Precautions:
- Insect Repellents: Essential for travelers to active CHIKV transmission areas.
- Long Sleeves and Pants: Minimize skin exposure.
- Screened Rooms: Ensure rooms are fitted with screens. Treatment for other health problem

Image by: yendex.com
WHO Response
The World Health Organization (WHO) plays a crucial role in responding to chikungunya:
- Outbreak Confirmation: Supports countries in confirming outbreaks through a network of laboratories.
- Technical Support: Provides guidance for effective management of mosquito-borne disease outbreaks.
- Tool Development: Reviews and supports the development of new tools for insecticide products and application technologies.
- Strategy Formulation: Formulates evidence-based strategies, policies, and outbreak management plans.
- Training: Offers training on clinical management, diagnosis, and vector control at the regional level.
- Guidelines and Handbooks: Publishes resources on epidemiological surveillance, laboratory, clinical case management, and vector control.
- Global Arbovirus Initiative: Advances integrated approaches across arboviral diseases through this initiative.
WHO encourages countries to build and maintain the capacity to detect and confirm cases, manage patients, and implement social communication strategies to reduce the presence of mosquito vectors.
Conclusion
Understanding chikungunya comprehensively is essential for effective prevention, management, and response. By implementing these measures, individuals, communities, and health organizations can collectively mitigate the impact of this mosquito-borne viral disease on public health.