The Impact of Climate Change on Infectious Diseases Climate change, a global phenomenon characterized by rising temperatures, shifting weather patterns, and increasing frequency of extreme weather events, has far-reaching consequences that extend beyond environmental degradation. One of the most pressing and often overlooked impacts of climate change is its influence on infectious diseases. This article
The Impact of Climate Change on Infectious Diseases
Climate change, a global phenomenon characterized by rising temperatures, shifting weather patterns, and increasing frequency of extreme weather events, has far-reaching consequences that extend beyond environmental degradation. One of the most pressing and often overlooked impacts of climate change is its influence on infectious diseases. This article delves into the intricate relationship between climate change and infectious diseases, exploring how alterations in our climate are reshaping the landscape of global health.
Climate Change and Its Mechanisms
Climate change refers to long-term shifts in temperature, precipitation, and other atmospheric conditions on Earth. These changes are primarily driven by human activities, particularly the burning of fossil fuels, deforestation, and industrial processes that release greenhouse gases like carbon dioxide and methane into the atmosphere. These gases trap heat, leading to a gradual warming of the planet.
The consequences of climate change are multifaceted, affecting various aspects of the environment and human life. Rising temperatures, altered precipitation patterns, and increased frequency of extreme weather events such as hurricanes, droughts, and floods are some of the most noticeable effects. These changes, in turn, create a cascade of impacts on ecosystems, agriculture, water resources, and human health.
The Nexus Between Climate Change and Infectious Diseases
Infectious diseases, caused by pathogens such as bacteria, viruses, fungi, and parasites, are highly sensitive to environmental conditions. Climate change influences the transmission dynamics, geographic distribution, and seasonality of these diseases in several ways:
- Vector-Borne Diseases: Many infectious diseases are transmitted by vectors, such as mosquitoes, ticks, and fleas. Climate change affects the habitats, life cycles, and population dynamics of these vectors. For instance, warmer temperatures can extend the breeding season and geographic range of mosquitoes, leading to the spread of diseases like malaria, dengue fever, and Zika virus to previously unaffected regions. Similarly, tick-borne diseases like Lyme disease are expanding their range as milder winters and longer summers create favorable conditions for tick survival.
- Water-Borne Diseases: Changes in precipitation patterns and increased frequency of extreme weather events can lead to contamination of water sources, promoting the spread of water-borne diseases. Heavy rainfall and flooding can overwhelm sanitation systems, leading to outbreaks of diseases like cholera, leptospirosis, and cryptosporidiosis. Conversely, droughts can reduce water availability, forcing people to rely on unsafe water sources, further increasing the risk of disease transmission.
- Food-Borne Diseases: Climate change can also impact food safety and security, influencing the incidence of food-borne diseases. Rising temperatures and changing weather patterns can affect crop yields, food storage, and distribution systems. Higher temperatures can promote the growth of foodborne pathogens like Salmonella and E. coli, while extreme weather events can disrupt food supply chains, leading to food shortages and malnutrition, which weaken immune systems and increase susceptibility to infections.
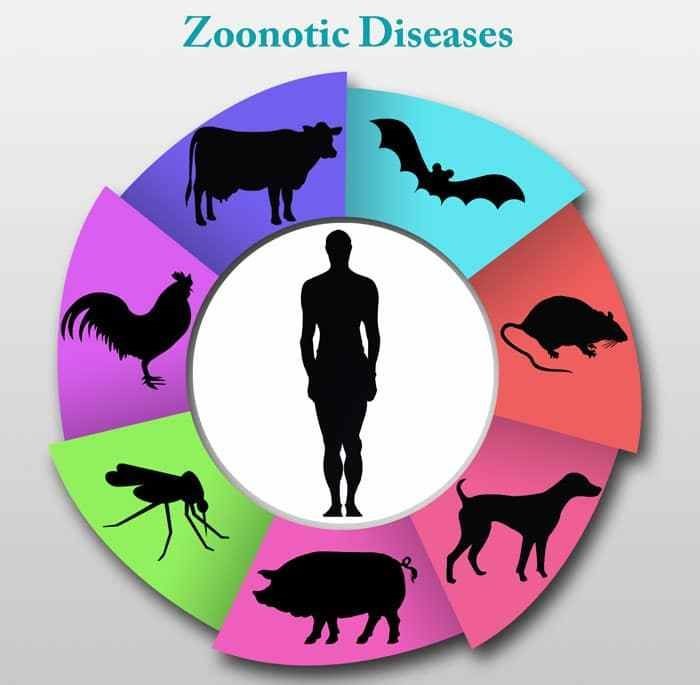
- Zoonotic Diseases: Climate change can alter the interactions between humans, animals, and their environments, increasing the risk of zoonotic diseases—those that are transmitted from animals to humans. Habitat destruction, changes in land use, and shifting wildlife populations can bring humans into closer contact with animals that harbor infectious agents. For example, deforestation and urbanization can lead to increased human exposure to bats and rodents, which are reservoirs for diseases like Ebola and hantavirus.
- Respiratory Infections: Climate change can exacerbate respiratory infections by affecting air quality and promoting the spread of respiratory pathogens. Increased temperatures can lead to higher levels of air pollution, including ground-level ozone and particulate matter, which can irritate the respiratory system and increase susceptibility to infections like influenza and pneumonia. Additionally, changes in humidity and temperature can influence the survival and transmission of respiratory viruses.
Picture by: Yandex.com
Case Studies and Examples
Several case studies illustrate the complex interplay between climate change and infectious diseases:
- Malaria: Malaria is a mosquito-borne disease that thrives in warm, humid environments. Climate change has expanded the range of malaria-carrying mosquitoes, leading to the re-emergence of malaria in areas where it was previously eradicated. For example, in the highland regions of East Africa, rising temperatures have allowed malaria-carrying mosquitoes to thrive at higher altitudes, putting previously unaffected populations at risk.
- Dengue Fever: Dengue fever, transmitted by Aedes mosquitoes, is another disease influenced by climate change. Warmer temperatures and increased rainfall create ideal breeding conditions for these mosquitoes. As a result, dengue fever has spread to new regions, including parts of the United States and Europe, where it was once rare.
- Cholera: Cholera, a water-borne disease caused by the bacterium Vibrio cholerae, is closely linked to environmental conditions. Climate change-induced flooding and extreme weather events can contaminate water sources with cholera bacteria. For instance, in 2010, a devastating cholera outbreak occurred in Haiti following a massive earthquake and subsequent flooding, highlighting the vulnerability of populations to water-borne diseases in the wake of climate-related disasters.
Mitigation and Adaptation Strategies
Addressing the impact of climate change on infectious diseases requires a multifaceted approach that combines mitigation and adaptation strategies:
- Mitigation: Reducing greenhouse gas emissions is crucial to slowing the pace of climate change and mitigating its impacts on infectious diseases. Transitioning to renewable energy sources, improving energy efficiency, and implementing sustainable land-use practices are essential steps in this direction.
- Surveillance and Early Warning Systems: Strengthening disease surveillance and early warning systems can help detect and respond to outbreaks of infectious diseases in a timely manner. Monitoring environmental conditions, vector populations, and disease incidence can provide valuable data for predicting and preventing outbreaks.
- Public Health Infrastructure: Investing in robust public health infrastructure is essential for managing the health impacts of climate change. This includes improving access to clean water and sanitation, enhancing healthcare facilities, and ensuring adequate resources for disease prevention and control.
- Community Engagement and Education: Raising awareness about the link between climate change and infectious diseases is vital for promoting community resilience. Educating communities about preventive measures, such as vector control, safe water practices, and hygiene, can empower individuals to protect themselves and their families.
- Research and Innovation: Continued research is needed to understand the complex interactions between climate change and infectious diseases. Developing innovative solutions, such as climate-resilient crops, vaccines, and vector control technologies, can help mitigate the health impacts of climate change.
Conclusion
Climate change is a global challenge with profound implications for public health, particularly in the realm of infectious diseases. The intricate relationship between climate change and infectious diseases underscores the need for comprehensive and coordinated efforts to address both issues simultaneously. By mitigating the drivers of climate change, strengthening public health infrastructure, and enhancing community resilience, we can better protect populations from the growing threat of climate-related infectious diseases. As we navigate the complexities of a changing climate, a proactive and informed approach will be essential to safeguarding global health in the years to come.